Tuberculosis And Covid-19: Fighting A Deadly Syndemic - Forbes

Kiran Sitaras on their mission of ending TB among their local community via door-to-door household ... [+]
Asad Zaidi, Interactive Research & Development, PakistanBefore Covid-19, there was a much older, deadly respiratory killer. It is called tuberculosis. Two years ago, on 26 September 2018, I had the opportunity to attend and speak at the first ever United Nations High Level Meeting (UNHLM) on Tuberculosis. I left the meeting excited and energized. After all, TB, an ancient but neglected epidemic, finally got noticed in a high-profile event, where country leaders acknowledged the enormous burden of TB, and pledged their commitment to ending the epidemic by 2030. The meeting resulted in ambitious targets and a political declaration.
This week, two years after the UNHLM, the World Health Organization and partners released a progress report, to take stock of progress made in meeting the Sustainable Development Goal (SDG) and UNHLM targets for TB. The news is not good.
Sadly, the report shows poor progress in meeting both SDG and UNHLM targets (infographic below). In 2019, 1.4 million people died of TB, and 10 million people developed the disease. While the target for TB preventive therapy is 30 million by 2022, only 6.3 million people have been treated during 2018 and 2019. While the target for funding TB care and prevention is $13 billion annually, only $6.5 billion were raised during 2020. By 2020, nobody should have faced catastrophic costs due to TB, but one in two people with TB still face such economic challenges.

Progress towards achieving global TB targets and implementation of the UN Political Declaration on ... [+]
World Health OrganizationSpeaking at the UNGA side event this week (video link below), where the two year progress report was released, WHO Director-General Dr Tedros Adhanom Ghebreyesus made a strong call to action. “Accelerated action is urgently needed worldwide, if we are to meet our targets by 2022,” he said. “The Covid-19 pandemic threatens to unwind the gains we have made. The impact of the pandemic on TB services has been severe,” he added.
Devastating impact of Covid-19 on TB services
Earlier this month, several civil society organizations working on TB released the results of a large survey done to document the impact of the pandemic on TB care, research and funding. The results are sobering (infographic below).
Around the world, policy and program officers reported significant drops in TB notification (88% in the Global Fund implementing countries and 68% in the USA). Over 70% of healthcare workers and advocates reported a decrease in the number of people coming to health facilities for TB testing. In Kenya, 50% of people with TB reported having trouble finding transport to care and in India, 36% of people with TB reported health facilities they normally visit closed.
"Findings of the report reinforce an urgent need for targeted investments in strengthening community responses to ending both Covid-19 and TB,” said Robyn Waite, a Policy and Advocacy Manager at Results Canada, one of the agencies that co-led the survey. “Now more than ever people must come together to share knowledge and information, pool resources, and coordinate effectively to maximize impact,” she added.
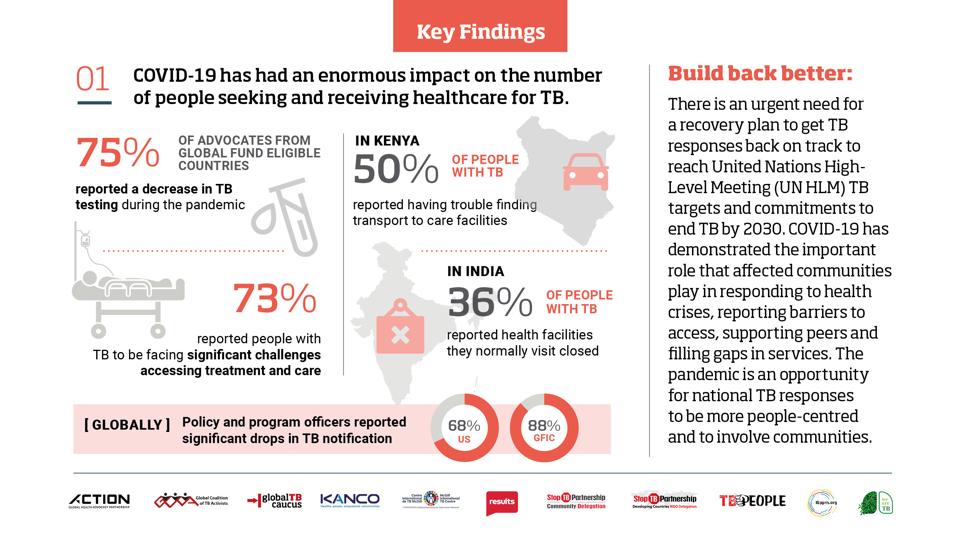
COVID-19 has had an enormous impact on the number of people seeking and receiving healthcare for TB ... [+]
Report: The impact of COVID-19 on the TB epidemic: A community perspectiveSimilar surveys by WHO and Global Fund confirm the widespread disruption of routine TB services. And mathematical models suggest that disruption of TB services might substantially increase TB mortality and incidence.
Speaking at the UNGA event, Dr Tereza Kasaeva, Director of WHO’s Global TB Programme, presented a WHO analysis on impact of COVID-19 on TB deaths. The model indicates that a 50% drop in TB case detection over 3 months could lead to an increase in the number of TB deaths worldwide by nearly 400,000 in 2020 alone.
Tackling the deadly syndemic
It is clear that current efforts to end TB are off-track. They were off-track even before Covid-19, and the pandemic has made things much harder. Together, Covid-19 and TB pose a deadly, dual threat - a syndemic that feeds on social inequities and poverty. Tremendous catch-up work, advocacy, and funding will be needed, to get back on track, even as the pandemic is pushing the world into the deepest recession since the second World War.
In the immediate term, all countries must identify TB patients who were missed during lock-downs, and make sure they get quality treatment. Ensuring continuity of TB services is critical. In the longer term, countries will have to address poverty and social determinants that include malnutrition, overcrowding, poor housing, and unemployment. During this crisis, over 37 million people have already been pushed into extreme poverty. History reminds us that TB and poverty are inseparable.
India, the world’s highest TB burden country, had a prolonged lock-down, and nearly half a million persons with TB have been missed during the past 6 months (60% drop in TB notifications, compared to 2019). Thousands of children have missed their BCG vaccine shots - 1 million fewer children got the vaccine during April 2020, as compared to January. India is now the epicenter of two deadly, respiratory infections. India is also facing a massive contraction of its economy, which, in turn, will worsen the TB epidemic in the country.
Ms Blessina Kumar, member of the WHO Civil Society Taskforce on TB and CEO of GCTA made a passionate call for greater investment, accountability and research to end TB especially in the face of the COVID-19 crisis. “Invest, invest, invest,” she said. “TB funding has reduced significantly, especially in the past 6-8 months, while at the same time billions of dollars have been made available for Covid-19. This is indeed great for Covid-19. But not at the cost of TB,” she argued. She pointed out that TB continues to be the biggest killer, even during Covid-19, and encouraged leaders to not shift their focus away from TB.

A woman TB champion is conducting household contact tracing and TB counselling in Yangon, Myanmar
Kyawzin Thann, PATH, MyanmarSo, how do countries get back on track? WHO and partners are urging countries to implement the following 10 priority recommendations to put the world on track to reach agreed targets by 2022 and beyond:
- Fully activate high-level leadership to urgently reduce TB deaths and drive multi-sectoral action to end TB
- Urgently increase funding for essential TB services including for the health workforce
- Advance universal health coverage to ensure all people with TB have access to affordable quality care and resolve under-reporting challenges
- Address the drug-resistant TB crisis to close persistent gaps in care
- Dramatically scale up provision of TB preventive treatment
- Promote human rights and combat stigma and discrimination
- Ensure meaningful engagement of civil society, communities and people affected by TB
- Substantially increase investments in TB research to drive technological breakthroughs and rapid uptake of innovations
- Ensure that TB prevention and care are safeguarded in the context of COVID-19 and other emerging threats
- Request WHO to continue to provide global leadership for the TB response, working in close collaboration with Member States and other stakeholders, including to prepare for a High-Level Meeting on TB in 2023
Yes, implementing these recommendations during this crisis, amidst a global economic recession, will not be easy. But all countries must dig deep and find new funds to deal with the Covid-19 crisis, and not take money away from TB or AIDS, or other health priorities. Countries must also use innovations and systems developed for one condition that can be leveraged for the other.
“The pandemic has set us back in the fight against TB,” said Dr Soumya Swaminathan, Chief Scientist at WHO. “We should leverage the innovations in the response to Covid-19 to address some long standing bottlenecks in TB diagnosis and management. For instance, there has been huge investment in development of rapid diagnostics, in contact tracing apps and other digital tools for e consultation and follow up. The use of masks is becoming more socially acceptable. People with fever and cough are being screened for Covid-19 and should be tested for TB too, where appropriate. And finally, we have demonstrated that with global solidarity, a lot can be achieved in a short time. Open data, open access research and (to some extent) pooling of technology have all become the norm and should be continued for global threats like TB,” she said.
Not a zero-sum game
Global health is not a zero-sum game. We need to urgently tackle the coronavirus pandemic, and simultaneous deal with other existing health priorities. We don’t need to pick one. And we cannot “Covidize” all research either. As I have argued earlier, all health research cannot be about a pandemic or infectious threats, and all infectious-disease research cannot be about Covid-19.
Diagnostic and pharma companies are all hyper-focused on Covid-19 right now. This is necessary, but, again, cannot come at the expense of manufacturing tests and medicines for TB, AIDS, malaria and other existing threats.
“Now that the world has witnessed how easily one infectious killer can affect millions, I hope more people will realize that TB is and will always be a major problem for us all,” says Zolelwa Sifumba, a South African physician who survived drug-resistant TB, and, more recently, had Covid-19 as well. “The very same urgency and actions we are taking against Covid-19 are needed against TB. It’s time for our leaders to recommit to the goals set two years ago. Action is needed now as we are losing the gains made and risk losing even more lives globally,” she added.
As a doctor in a small rural hospital in South Africa, Sifumba is living through the Covid-19 crisis and bearing witness to it’s impact on all other medical services, and on the economy. Indeed, if there is one lesson this pandemic has taught us, it is that investing in health is not a luxury. It is an essential, basic human right, and the world’s economy depends on health.

Comments
Post a Comment