FNB Infectious Disease: Admissions, medical colleges, fees, eligibility criteria details
What To Know About Infectious Colitis
Infectious colitis is an inflammatory condition that can cause diarrhea. Treatment depends on whether the colitis results from bacteria, a virus, or a parasite.
Infectious colitis causes symptoms similar to inflammatory bowel disease (IBD), including rectal pain, increased urgency to pass stool, and bloody mucus discharge from the anus.
Several pathogens may cause this acute form of diarrhea, including viruses, parasites, and bacteria.
This article reviews what infectious colitis is, its types, symptoms, causes, and more.
Colitis is inflammation of the colon, which is the part of the intestines where stool forms.
Colitis can cause several symptoms, including:
Infectious colitis is a type of colitis resulting from viruses, bacteria, or parasites.
It is generally an acute illness that will clear within about 7 days, with or without treatment. More severe cases can last for several weeks.
Common types of colitis and their causes include:
While different types of colitis can cause similar symptoms, the underlying cause may affect treatment.
Infectious colitis can cause symptoms similar to those of IBD and gastroenteritis, such as:
Most people who develop infectious colitis do so after coming into contact with contaminated food or water.
People may be at higher risk of contracting infectious colitis if they:
Bacterial infections account for about 47% of all cases. Common bacterial causes in the United States include Salmonella and Clostridium difficile, also known as Clostridioides difficile.
Living with certain medical conditions, such as sickle cell anemia or hemolytic anemia, or taking certain medications, such as immunosuppressors, puts a person at a higher risk of Salmonella infection.
Other possible bacterial causes include:
Less commonly, amebic (parasitic) and viral infections can cause colitis.
During an exam, a doctor will ask about a person's symptoms. They may also ask about possible exposure to known risk factors, such as a recent hospital stay or travel abroad.
They will likely run bacteria cultures of stool samples to determine whether the underlying cause of symptoms is bacterial in origin.
The doctor may also order additional testing, such as CT scans, a colonoscopy, tissue biopsies, and fecal cultures, to rule out other colitis causes.
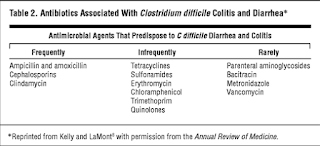
Treatment may vary depending on the cause. Antibiotics can help treat bacterial colitis. However, antibiotics are inappropriate for children because of the risk of hemolytic uremic syndrome.
For C. Diff, doctors recommend antibiotic treatment for most people, especially if they are immunosuppressed.
Most people with mild forms of colitis do not need treatment. Infections typically clear on their own.
A person may develop dehydration due to fluid loss from diarrhea.
Other complications depend on the underlying pathogen causing the infection. Possible complications include:
Most cases of infectious colitis will clear in about 7 days. However, in severe cases, it may take several weeks before the infection clears.
In some cases, a person can contract the infection again shortly after infection — for example, about 1 in 6 people with C. Diff get it again within the following 2–8 weeks. Washing hands regularly, sanitizing surfaces, and avoiding people with the infection can help prevent a recurrence.
In addition to antibiotic treatment, in some cases, a fecal transplant may be necessary.
Below are some common questions on infectious colitis.
How serious is infectious colitis and how long does it last?Most people start to feel better in about 7 days. In severe cases, it can take several weeks before the infection passes.
How do you get a colitis infection?The most common form of transmission is through contaminated food or water.
What is the treatment for infectious colitis?Treatments may involve letting the infection run its course or providing fluids and antibiotics. Some people may need fluids in a hospital setting.
What is the difference between infectious and ulcerative colitis?Ulcerative colitis is a type of chronic inflammatory bowel disease. It results from an abnormal immune response where the immune system attacks healthy colon tissue.
Infectious colitis results from an infectious agent that causes inflammation in the colon. It is generally self-limiting and clears within a few days.
What is the difference between infectious colitis and gastroenteritis?Gastroenteritis occurs due to a viral or bacterial infection, commonly rotavirus. It is common in children. Similar to infectious colitis, it causes intestinal inflammation, but it also causes inflammation in the stomach.
Another main difference is that gastroenteritis typically does not cause bloody diarrhea.
Infectious colitis is inflammation of the intestines resulting from an underlying bacterial, viral, or parasitic infection. Bacteria are the most common cause of infectious colitis.
Generally, the condition does not require medical treatment.
Some people may contract the infection again. Regular handwashing and avoiding those with an infection can help prevent reinfection.
Inflammatory Bowel Disease: Symptoms And Treatment
SOURCES:
National Digestive Diseases Information Clearinghouse, National Institutes of Health.
FDA: "FDA approves Inflectra, a biosimilar to Remicade," "FDA approves Amjevita, a biosimilar to Humira."
Crohn's & Colitis Foundation of America: "Maintenance Therapy," "What is Crohn's Disease?" "What is Ulcerative Colitis?"
Mayo Clinic.
University of Maryland Medical Center.
Faten Aberra, MD, assistant professor of medicine, gastroenterology division, University of Pennsylvania.
Raymond K. Cross Jr., MD, professor of medicine, gastroenterology division, University of Maryland School of Medicine.
Kristen Farwell, MD, gastroenterologist, Lahey Hospital & Medical Center, Burlington, MA.
Edward V. Loftus Jr., MD, professor of medicine, division of gastroenterology and hepatology, Mayo Clinic, Rochester, MN.
Overprescribed Antibiotics For Colds Causes Patient Harm
THURSDAY, April 27, 2023 (HealthDay News) — Overprescribing of antibiotics for acute upper respiratory infections (aURIs) causes significant patient harm, according to a study published in the April issue of the Journal of Internal Medicine.
Harris Carmichael, M.D., from the Stanford University School of Medicine in California, and colleagues analyzed data from 51 million patient encounters to determine the odds of clinically detectable adverse events following antibiotic use compared with events among unexposed individuals with aURIs.
The researchers found that 62.4 percent of the population received antibiotics in an aURI encounter. In the antibiotic-exposed group, observed adverse events included 54,279 for diarrhea and 46,936 for candidiasis (adjusted odds ratios [aORs], 1.24 and 1.61, respectively; number needed to harm: 3,126 and 1,975, respectively). For Clostridium difficile infection (CDI), the exposed group had 30,133 observed events (aORs of isolated CDI and combined adverse events were 1.07 and 1.30, respectively; number needed to harm: 17,695 and 1,150, respectively). Adverse events were more common among females. Following a URI, antibiotics resulted in 5.7 additional cases of CDI per 100,000 outpatient prescriptions.
"These findings underscore that inappropriately giving patients antibiotics is causing real and widespread harm," Carmichael said in a statement. "Having these kinds of side effects for one in a few hundred, or even a thousand, patients may not seem like a lot, but when you look at this problem on a population health level, we're talking about hundreds of thousands of adverse events severe enough that these patients needed additional care from a doctor."
Abstract/Full Text (subscription or payment may be required)
Copyright © 2023 HealthDay. All rights reserved.

Comments
Post a Comment