Cutaneous Manifestations of HIV: Overview, Manifestations by HIV Disease Stage, Manifestations in HIV-Infected ...
Everything You Need To Know About Pneumonia
Pneumonia is an infection caused by bacteria, viruses, or fungi. It leads to inflammation in the air sacs of one or both lungs. These sacs, called alveoli, fill with fluid or pus, making it difficult to breathe.
Both viral and bacterial pneumonia is contagious. This means they can spread from person to person through inhalation of airborne droplets from a sneeze or cough.
You can also get these types of pneumonia by coming into contact with surfaces or objects that are contaminated with pneumonia-causing bacteria or viruses.
You can contract fungal pneumonia from the environment. It does not spread from person to person.
Pneumonia is further classified according to where or how it was acquired:
Walking pneumonia is a milder case of pneumonia. People with walking pneumonia may not even know they have pneumonia. Their symptoms may feel more like a mild respiratory infection than pneumonia. However, walking pneumonia may require a longer recovery period.
The symptoms of walking pneumonia can include things like:
Viruses and bacteria, like Streptococcus pneumoniae or Haemophilus influenzae, often cause pneumonia. However, in walking pneumonia, the bacteria Mycoplasma pneumoniae most commonly causes the condition.
Learn more about pneumonia during pregancy (maternal pneumonia).
Pneumonia may be classified based off the area of the lungs it's affecting:
BronchopneumoniaBronchopneumonia can affect areas throughout both of your lungs. It's often localized close to or around your bronchi. These are the tubes that lead from your windpipe to your lungs.
Lobar pneumoniaLobar pneumonia affects one or more lobes of your lungs. Each lung is made of lobes, which are defined sections of the lung.
Lobar pneumonia can be further divided into four stages based off how it's progressed:
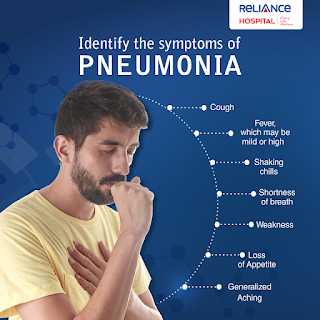
Pneumonia symptoms can be mild to life threatening. They can include:
Other symptoms can vary according to your age and general health:
Pneumonia happens when germs get into your lungs and cause an infection. The immune system's reaction to clear the infection results in inflammation of the lung's air sacs (alveoli). This inflammation can eventually cause the air sacs to fill up with pus and liquids, causing pneumonia symptoms.
Several types of infectious agents can cause pneumonia, including bacteria, viruses, and fungi.
Bacterial pneumoniaThe most common cause of bacterial pneumonia is Streptococcus pneumoniae. Other causes include:
Viral pneumoniaRespiratory viruses are often the cause of pneumonia. Examples of viral infections that can cause pneumonia include:
Although the symptoms of viral and bacterial pneumonia are very similar, viral pneumonia is usually milder. It can improve in 1 to 3 weeks without treatment.
According to the National Heart, Lung, and Blood Institute, people with viral pneumonia are at risk of developing bacterial pneumonia.
Fungal pneumoniaFungi from soil or bird droppings can cause pneumonia. They most often cause pneumonia in people with weakened immune systems. Examples of fungi that can cause pneumonia include:
Anyone can get pneumonia, but certain groups do have a higher risk. These groups include:
Your doctor will start by taking your medical history. They'll ask you questions about when your symptoms first appeared and your health in general.
They'll then give you a physical exam. This will include listening to your lungs with a stethoscope for any abnormal sounds, such as crackling.
Depending on the severity of your symptoms and your risk of complications, your doctor may also order one or more of these tests:
Chest X-rayAn X-ray helps your doctor look for signs of inflammation in your chest. If inflammation is present, the X-ray can also inform your doctor about its location and extent.
Blood cultureThis test uses a blood sample to confirm an infection. Culturing can also help identify what may be causing your condition.
Sputum cultureDuring a sputum culture, a sample of mucus is collected after you've coughed deeply. It's then sent to a lab to be analyzed to identify the cause of the infection.
Pulse oximetryA pulse oximetry measures the amount of oxygen in your blood. A sensor placed on one of your fingers can indicate whether your lungs are moving enough oxygen through your bloodstream.
CT scanCT scans provide a clearer and more detailed picture of your lungs.
Fluid sampleIf your doctor suspects there's fluid in the pleural space of your chest, they may take a fluid sample using a needle placed between your ribs. This test can help identify the cause of your infection.
BronchoscopyA bronchoscopy looks into the airways in your lungs. It does this using a camera on the end of a flexible tube that's gently guided down your throat and into your lungs.
Your doctor may do this test if your initial symptoms are severe, or if you're hospitalized and not responding well to antibiotics.
If you need help finding a primary care doctor, then check out our FindCare tool here.
Your treatment will depend on the type of pneumonia you have, how severe it is, and your general health.
Prescription medicationsYour doctor may prescribe a medication to help treat your pneumonia. What you're prescribed will depend on the specific cause of your pneumonia.
Oral antibiotics can treat most cases of bacterial pneumonia. Always take your entire course of antibiotics, even if you begin to feel better. Not doing so can prevent the infection from clearing, and it may be harder to treat in the future.
Antibiotic medications don't work on viruses. In some cases, your doctor may prescribe an antiviral. However, many cases of viral pneumonia clear on their own with at-home care.
Antifungal medications are used to treat fungal pneumonia. You may have to take this medication for several weeks to clear the infection.
OTC medicationsYour doctor may also recommend over-the-counter (OTC) medications to relieve your pain and fever, as needed. These may include:
Your doctor may also recommend cough medicine to calm your cough so you can rest. Keep in mind coughing helps remove fluid from your lungs, so you don't want to eliminate it entirely.
Home remediesAlthough home remedies don't actually treat pneumonia, there are some things you can do to help ease symptoms.
Coughing is one of the most common symptoms of pneumonia. Natural ways to relieve a cough include gargling salt water or drinking peppermint tea.
Cool compresses can work to relieve a fever. Drinking warm water or having a nice warm bowl of soup can help with chills. Here are more home remedies to try.
You can help your recovery and prevent a recurrence by getting a lot of rest and drinking plenty of fluids.
Although home remedies can help ease symptoms, it's important to stick to your treatment plan. Take any prescribed medications as directed.
HospitalizationIf your symptoms are very severe or you have other health problems, you may need to be hospitalized. At the hospital, doctors can keep track of your heart rate, temperature, and breathing. Hospital treatment may include:
Pneumonia may cause complications, especially in people with weakened immune systems or chronic conditions, such as diabetes.
Complications may include:
In many cases, pneumonia can be prevented.
VaccinationThe first line of defense against pneumonia is to get vaccinated. There are several vaccines that can help prevent pneumonia.
Prevnar 13 and Pneumovax 23These two pneumonia vaccines help protect against pneumonia and meningitis caused by pneumococcal bacteria. Your doctor can tell you which one might be better for you.
Prevnar 13 is effective against 13 types of pneumococcal bacteria. The CDC recommends this vaccine for:
Pneumovax 23 is effective against 23 types of pneumococcal bacteria. The CDC recommends it for:
Pneumonia can often be a complication of the flu, so be sure to also get an annual flu shot. The CDC recommends that everyone ages 6 months and older get vaccinated, particularly those who may be at risk of flu complications.
Covid vaccineCOVID-19 can lead to pneumonia. The CDC recommends that everyone 6 months and older should receive an updated COVID-19 vaccine.
Hib vaccineThis vaccine protects against Haemophilus influenzae type b (Hib), a type of bacterium that can cause pneumonia and meningitis. The CDC recommends this vaccine for:
According to the National Heart, Lung, and Blood Institute, pneumonia vaccines won't prevent all cases of the condition.
But if you're vaccinated, you're likely to have a milder and shorter illness as well as a lower risk of complications.
Other prevention tipsIn addition to vaccination, there are other things you can do to avoid pneumonia:
Together with vaccination and additional prevention steps, you can help reduce your risk of getting pneumonia. Here are even more prevention tips.
A variety of infectious agents cause pneumonia. With proper recognition and treatment, many cases of pneumonia can be cleared without complications.
For bacterial infections, stopping your antibiotics early can cause the infection to not clear completely. This means your pneumonia could come back.
Stopping antibiotics early can also contribute to antibiotic resistance. Antibiotic-resistant infections are more difficult to treat.
Viral pneumonia often resolves in 1 to 3 weeks with at-home treatment. In some cases, you may need antivirals.
Antifungal medications treat fungal pneumonia. It may require a longer period of treatment.
Pneumonia can become dangerous quickly, particularly in young children. Here's how to avoid complications.
Most people respond to treatment and recover from pneumonia. Like your treatment, your recovery time will depend on the type of pneumonia you have, how severe it is, and your general health.
A younger person may feel back to normal in a week after treatment. Others may take longer to recover and may have lingering fatigue. If your symptoms are severe, your recovery may take several weeks.
Consider taking these steps to aid in your recovery and help prevent complications from occurring:
Pneumonia is a lung infection caused by bacteria, viruses, or fungi. The immune system's reaction to this infection causes the lung's air sacs to fill with pus and fluids. This leads to symptoms such as trouble breathing, a cough with or without mucus, fever, and chills.
To diagnose pneumonia, your doctor will do a physical exam and discuss your medical history. They may recommend further testing, such as a chest X-ray.
Treatment depends on the cause of the infection. It may involve antibiotics, antiviral medication, or antifungal medication.
Pneumonia often clears up in a few weeks. See a doctor right away if your symptoms get worse, as you may need to be hospitalized to prevent or treat more serious complications.
Deadly Diseases
The Greek physician Hippocrates described the symptoms of pneumonia 2,400 years ago. But this affliction of the lungs still kills more people in the United States than any other infectious disease, taking 40,000 to 70,000 lives each year. It is the most common lethal nosocomial, or hospital-acquired, infection.
The term "pneumonia" describes a group of symptoms that may be caused by bacteria, viruses, parasites, or fungi. Pneumonia is a severe inflammation of the lungs in which the thin tissue around air spaces called alveoli swells and fills with fluid. Symptoms include shaking, chills, a rapidly rising fever, and sharp chest pain made worse by breathing and coughing. Pneumonia is a common cause of death among elderly people and young children whose immune systems are weakened or impaired in some way.
A common bacterium, Streptococcus pneumoniae, lives in the respiratory tract of 15 percent of the population without causing problems. It can spread pneumonia only if inhaled deeply into the lungs. The germ travels via droplets conveyed through coughing, sneezing, and even talking in close proximity. Bacterial pneumonia is most common in winter and spring, when upper respiratory tract infections are frequent. Pneumonia is also a common complication of influenza.
Most cases of bacterial pneumonia can be effectively treated with penicillin. Between 1936 and 1945, pneumonia death rates in the United States dropped approximately 40 percent with the greater availability of antibiotics. The more common viral pneumonia usually diminishes on its own, but all strains of pneumonia can be serious if neglected, and people should always seek medical supervision for their care.
Along with other acute respiratory infections, pneumonia is in a near tie with diarrheal diseases as a leading cause of death in children under 5 worldwide. It's estimated that pneumonia kills approximately two million children each year, with 40 percent of these deaths in Africa. More than two-thirds of pneumonia deaths among children in the developing world are caused by just two kinds of bacteria: Pneumoccoccus and Hemophilus influenzae.
Trained community health workers can dramatically reduce these deaths when they teach parents to identify the early signs of pneumonia: rapid breathing and violent shaking in the chest. At present, as many as two-thirds of children with acute respiratory infections are not treated by trained health providers. Even the simplest understanding of how to count the number of breaths a child takes per minute can help community health workers and parents recognize pneumonia and administer antibiotics if appropriate, or seek help at a clinic or hospital.
Time is often of the essence with pneumonia: Severe pneumonia can kill victims within hours as they literally drown in the fluids flooding their lungs. In Honduras, pneumonia treatment is part of a national, integrated community child care program that trains community volunteers to monitor children's growth, provide health education, and treat pneumonia and diarrhea.
A major contributing factor to respiratory infections is indoor air pollution. We tend to think of this type of air pollution as a problem in the industrialized world, but half of the world's people rely on dung, wood, crop waste, or coal for cooking and heating. These solid fuels cause high levels of particulate matter in the developing world that are 100 times higher than concentrations in the United States or Europe. Poor ventilation of smoke makes breathing difficult and exposes young children to severe respiratory infections. Reducing indoor air pollution may require switching to cleaner and more efficient fuels such as liquid petroleum, electricity, or solar power, and the cooperation of governments. Pneumonia is also a leading cause of immediate death among AIDS patients.
Vaccines against certain kinds of pneumonia exist for adults, but many high-risk patients do not routinely receive them. A relatively new pneumococcal vaccine for children called Prevnar, introduced by Wyeth Pharmaceuticals, has proved effective in the United States, dramatically reducing disease incidence by approximately 80 percent. But the $50-per-dose U.S. Price makes it far too expensive to be widely used in the developing world. Another H Flu (Hib) vaccine has also been found to be effective in field testing. International health economists are searching for a better way to fund lifesaving vaccines than relying on the free market alone.
Return to Deadly Diseases
'Walking Pneumonia' Surge Observed At Cook Children's
Cook Children's Hospital in Fort Worth, Texas, began seeing a rise of mycoplasma pneumonia in patients in April, and since then, they've unexpectedly increased.
As of late June, the hospital had 80 positive cases out of 398 patients — almost a 20% positivity rate systemwide, it reported July 1. Last year, during the same time frame, the hospital had 0 cases of what's also commonly called "walking pneumonia", according to the news release.
"This is a really common bacterial infection that's been around for a long time," Nicholas Rister, MD, a physician at Cook Children's Infectious Disease - Dodson Specialty Clinics, said in an accompanying video announcement. "We've just been seeing really elevated rates of it in our community over the past month."
Mycoplasma pneumonia can spread through the air via coughing or sneezing and in a small percentage of cases, hospitalization can be necessary.
"When people need hospital care due to pneumonia, M. Pneumoniae are a common bacterial cause of the infection," according to the CDC. "For children, they're the most common cause."
The bacteria can take between one and four weeks for symptoms to begin after exposure, if infected.
The most at-risk group for infections are school age children and young adults, and this year, Cook Children's is seeing infections across a span of ages, it reported.
Infection can be prevented with handwashing and hygiene, but there is no vaccine for M. Pneumonia currently.


Comments
Post a Comment