Majocchi's granuloma: current perspectives | IDR
What To Know About Bacterial Skin Infections
Bacterial skin infections occur when bacteria enter through the surface of the skin. They can cause symptoms such as swelling and inflammation. Treatment may include topical or oral antibiotics.
Experts classify bacterial skin infections as skin and soft tissue infections (SSTI) or acute bacterial skin and skin structure infections (ABSSSI).
This article details the types of bacterial skin infections and discusses symptoms, causes, treatment options, and more.
Skin infections involving bacteria can affect the skin, underlying subcutaneous tissue, or muscles, ranging from superficial surface infections to severe necrotizing conditions.
SSTIs are infections that affect the skin or soft tissue. The Food and Drug Administration (FDA) previously categorized these as "complicated SSTI" and "uncomplicated SSTI." More recently, the FDA has categorized bacterial skin infections as either SSTI or ABSSSI.
SSTIExamples of SSTI include:
ABSSSIABSSSIs are more complex bacterial skin infections. A 2013 FDA release defines ABSSSI as the following:
The primary infections in SSTIs are Streptococcus and Staphylococcus species, including methicillin-resistant Staphylococcus aureus (MRSA).
According to the Centers for Disease Control and Prevention (CDC), around 33% of people carry S. Aureus bacteria in their nose. Around 2 per 100 people carry MRSA. However, most people do not develop serious MRSA infections.
The CDC also reports that MRSA bloodstream infections decreased in healthcare settings by 17.1% each year between 2005–2012.
Learn more about MRSA.
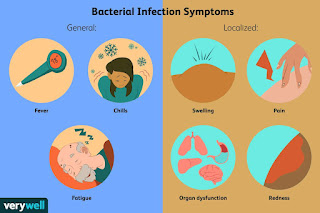
Symptoms of bacterial skin infections may depend on the type of infection but can include:
It is best for a person with any of these symptoms to contact a doctor for a diagnosis. A doctor can order tests to confirm the cause of the symptoms and advise on suitable treatments.
Learn more about the symptoms of a bacterial infection.
Bacterial skin infections can develop when bacteria enter through the surface of the skin. For example, this can happen through a cut or a wound.
Bacteria can also enter the skin through surgical incisions. As a result, SSTIs are the most common healthcare-associated infections among people undergoing surgery.
A doctor may diagnose a bacterial skin infection through clinical signs and symptoms.
They may also order laboratory tests to confirm the type of infection. This involves either swabbing or removing a sample of the affected skin for examination under a microscope.
A doctor can advise which tests they order and what the person can expect.
Experts recommend that doctors manage infections such as impetigo, erysipelas, and cellulitis with topical antibiotics against Gram-positive bacteria. Doctors may also treat community-acquired MRSA with antibiotics.
Additionally, medical professionals may treat simple abscesses and boils by making a surgical incision and draining them of pus.
In some cases, doctors may treat severe bacterial skin infections in hospitals. A person may require oral or intravenous antibiotics.
Learn more about antibiotics.
A person can take steps to reduce the risk of bacterial skin infections. These can include:
Guidelines recommend that medical staff take appropriate precautions to avoid bacterial skin infections in a hospital setting. Recommendations include ensuring that a person bathes or showers before surgery and that surgical teams clean their hands appropriately.
It is best for a person to contact their doctor for more advice on ways to prevent bacterial skin infections.
Bacterial skin infections comprise skin and soft tissue infections (SSTI) or acute bacterial skin and skin structure infections (ABSSSI). Symptoms can vary depending on the severity of the infection but can include inflammation, swelling, pain, and warmth.
Treatment for bacterial skin infections may involve topical medications to apply to the skin or oral antibiotics. For more severe conditions, doctors may administer antibiotics intravenously.
A person can help reduce the risk of bacterial skin infections. These include regularly washing hands and properly cleaning any cuts. It is best to contact a doctor for advice if a person has concerns about bacterial skin infections.
Prostatitis: What It Is, Symptoms, Causes And Treatment
When most men think about their prostate, it's to worry about whether they have prostate cancer or not. But another condition is far more common and plenty painful.
Prostatitis involves inflammation of the prostate gland and sometimes the areas around it. Not only is prostatitis highly treatable, but it is highly prevalent among men. According to the Prostate Cancer Foundation, it is the leading cause of urinary tract infections in men, resulting in approximately 2 million doctor's visits each year in the United States. In fact, it's estimated that half of all men will experience prostatitis at some point.
The U.S. National Center for Health Statistics further reveals that about 25% of men who seek medical attention for urological problems exhibit symptoms of prostatitis. Here, experts give the rundown on prostatitis, including its various types, causes, common symptoms and available treatments.
What is prostatitis?Prostatitis, a condition characterized by the inflammation of the prostate gland, is known for its frequent and often debilitating pain. According to the Cleveland Clinic, it is a complex condition that can lead to various symptoms, including infection, inflammation and pain.
Two types of prostatitis are associated with urinary tract infections (UTIs), while the remaining types may not have an infectious origin. Regardless of the type, prostatitis is commonly recognized for the intense pain its sufferers feel, which can significantly impact a man's quality of life.
Types of prostatitisAccording to the U.S. National Institute of Diabetes and Digestive and Kidney Diseases, there are four distinct types of prostatitis, each with its own characteristics:
Prostatitis causesAccording to the U.S. National Institutes of Health, the causes of prostatitis vary depending on the specific type of the condition:
It's important to know that acute bacterial prostatitis can be caused by various types of bacteria commonly associated with urinary tract infections. Additionally, prostatitis can also result from infections transmitted through sexual contact.
However, "you don't need to avoid sex if you have prostatitis. Typically, sex won't worsen prostatitis. But some men who have prostatitis have pain with ejaculation," Dr. Patricio Gargollo, a urologist with the Mayo Clinic, said in a recent article.
Prostatitis symptomsProstatitis has many symptoms that can significantly impact a man's daily life and well-being, especially when left untreated. Here are some common symptoms associated with prostatitis, according to Johns Hopkins Medicine:
Also, the symptoms of prostatitis can mimic those of other medical conditions or issues. Therefore, seeking medical advice from a health care provider for an accurate diagnosis is important.
Prostatitis treatmentThe treatment for prostatitis is determined by age, overall health, medical history, the severity of the condition, individual tolerance for specific treatments, expected duration and patient preference. The specific type of prostatitis also plays a significant role in determining the appropriate treatment. Here are some general treatment options for prostatitis, followed by specific treatments based on the different types of prostatitis.
Treatment for prostatitis typically involves a combination of approaches to relieve symptoms, eliminate infection (if present), reduce inflammation and improve overall prostate health. These may include:
But more specifically, the type of treatment recommended is typically based on the different types of prostatitis. Johns Hopkins Medicine indicates typical treatments for prostatitis as follows:
Copyright © 2023 HealthDay. All rights reserved.
Citation: Prostatitis: What it is, symptoms, causes and treatment (2023, May 31) retrieved 31 May 2023 from https://medicalxpress.Com/news/2023-05-prostatitis-symptoms-treatment.Html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without the written permission. The content is provided for information purposes only.
Fungal Meningitis Outbreak In Mexico Kills 2 After Cosmetic Surgeries. Here's What We Know—And Symptoms And Treatment.
ToplineA probable outbreak of fungal meningitis—an infection that causes inflammation near the brain and spinal cord—in Mexican medical clinics has left two Americans dead and over 200 infected, causing the U.S. And Mexico to ask the World Health Organization to issue a public health emergency declaration.
© Provided by Forbes Photomicrograph of mild meningitis along with hemorrhage, and the presence of Bacillus anthracis. Getty Images Key FactsThe Centers for Disease Control and Prevention announced two Americans have died from suspected cases of fungal meningitis and at least 220 others have been infected following an outbreak of the infection among patients who had surgery in Matamoros, Mexico.
According to the CDC, the outbreak was spread via epidural anesthesia (a procedure used to numb parts of the body by injecting anesthetic into a space next to the spinal cord) given to patients before surgery, and was associated with two clinics in the border city of Matamoros—River Side Surgical Center and Clinica K-3—that shut down on May 13.
Dallas Smith, a CDC epidemiologist, said in a webinar Friday that out of 10 possible cases, 100% of the patients received liposuction under epidural, 40% received breast augmentation and 30% got Brazilian butt lifts.
Smith also mentioned in the webinar that 205 of those exposed were women and 16 were men. The average age of the patients was 32, and 178 were from Texas.
The agency urges anyone who was administered epidural anesthesia at either of these clinics between January 1 and May 13 to seek immediate medical treatment—according to Mexico's Ministry of Health, around 547 people have surgery at the two clinics over that period.
The CDC has since placed Matamoros, Mexico on a level two travel advisory, cautioning Americans to practice enhanced precautions, like canceling any medical procedures that involve an epidural injection until there's no longer a risk.
U.S. And Mexican authorities have asked the World Health Organization to declare a public health emergency in response to the outbreak, which is meant to accelerate funding, treatment and international collaboration.
Key BackgroundMeningitis is the inflammation of the protective membranes covering the brain and spinal cord and can be caused by fungi, bacteria, viruses, amebas or parasites. There are six types of meningitis with varying levels of severity, and according to WHO, bacterial meningitis is the greatest concern. One in six people who get bacterial meningitis die, and one in five have severe complications.
Types Of MeningitisAccording to the Mayo Clinic, it can take weeks for symptoms to appear. Early meningitis symptoms for people two years and older resemble flu-like symptoms and include fever, nausea or vomiting, severe headaches, stiff neck, trouble sleeping, loss of appetite or thirst, seizures, trouble walking, confusion or trouble concentrating and rashes. Symptoms present slightly differently in infants and include fever, constant crying, irritability or trouble sleeping, vomiting, poor feeding, stiffness in the neck or body, not waking to eat and a bulge in the soft spot on top of the head. Medical attention is recommended if a patient develops a fever, stiff neck, confusion, vomiting or a severe headache that doesn't go away.
TangentMatamoros is a popular medical tourist destination, especially for U.S. Patients. A study published in Infection Control & Hospital Epidemiology found Mexico was the most common destination of choice for Americans seeking medical tourism, accounting for 41% of all visits. The study also reports dental work accounts for 55% of all treatment, though cosmetic surgeries, cancer care, fertility treatments and organ transplants are all popular among Americans seeking treatment abroad. Cost is typically the main reason for medical tourism—a 2020 study found 92% participants cited low cost in Mexico as a driving factor. However, the State Department recommends against traveling to the border state of Tamaulipas—home to Matamoros—due to rampant violence: In March, four Americans who traveled there for surgery were kidnapped by a suspected Mexican cartel, two of whom died.
Further ReadingMedical Tourism: The Benefits And Risks Of Getting A Tummy Tuck In Mexico Or IVF In India (Forbes)
Two Americans Dead And Two Others Found Alive After Violent Kidnapping In Mexico (Forbes)
U.S., Mexico ask WHO for emergency declaration over deadly fungal outbreak (CBS News)


Comments
Post a Comment